What Is PBA?
If you have been diagnosed with a neurologic condition or brain injury and have noticed changes in your crying and/or laughing, you may be experiencing Pseudobulbar Affect (PBA). PBA is a medical condition that causes crying and/or laughing that is sudden, frequent, uncontrollable and is exaggerated or doesn’t match how you feel. PBA may be caused by neurological damage related to your neurologic condition or brain injury but is a separate and treatable condition.
Some of the other ways that patients have described their crying and/or laughing episodes include:
- “Happens out of nowhere.”
- “Occurs for no good reason or without any warning.”
- “It’s very embarrassing.”
- “Feels like an overreaction.”
- “Can’t stop the episode even though I want to.”
- “I don’t know why the episode is happening.”
Signs and Symptoms of PBA
PBA symptoms have certain characteristics that help doctors distinguish it from other conditions. How you describe your episodes may help your doctor identify what is causing your episodes. Common characteristics that help differentiate PBA symptoms from other forms of crying and laughing can include any or all of the following:
Individual patients may have different experiences with their PBA symptoms, which can range from mild to severe. Some patients will experience only crying episodes, while others only laughing episodes, and some people may have both crying and laughing episodes.
The uncontrolled nature of PBA can be upsetting, uncomfortable, and embarrassing for the patient experiencing it. In addition, people who witness these expressions of crying and/or laughing may perceive them as being unreasonable and disconnected from the situation.
PBA Is Neurological, Not Psychological
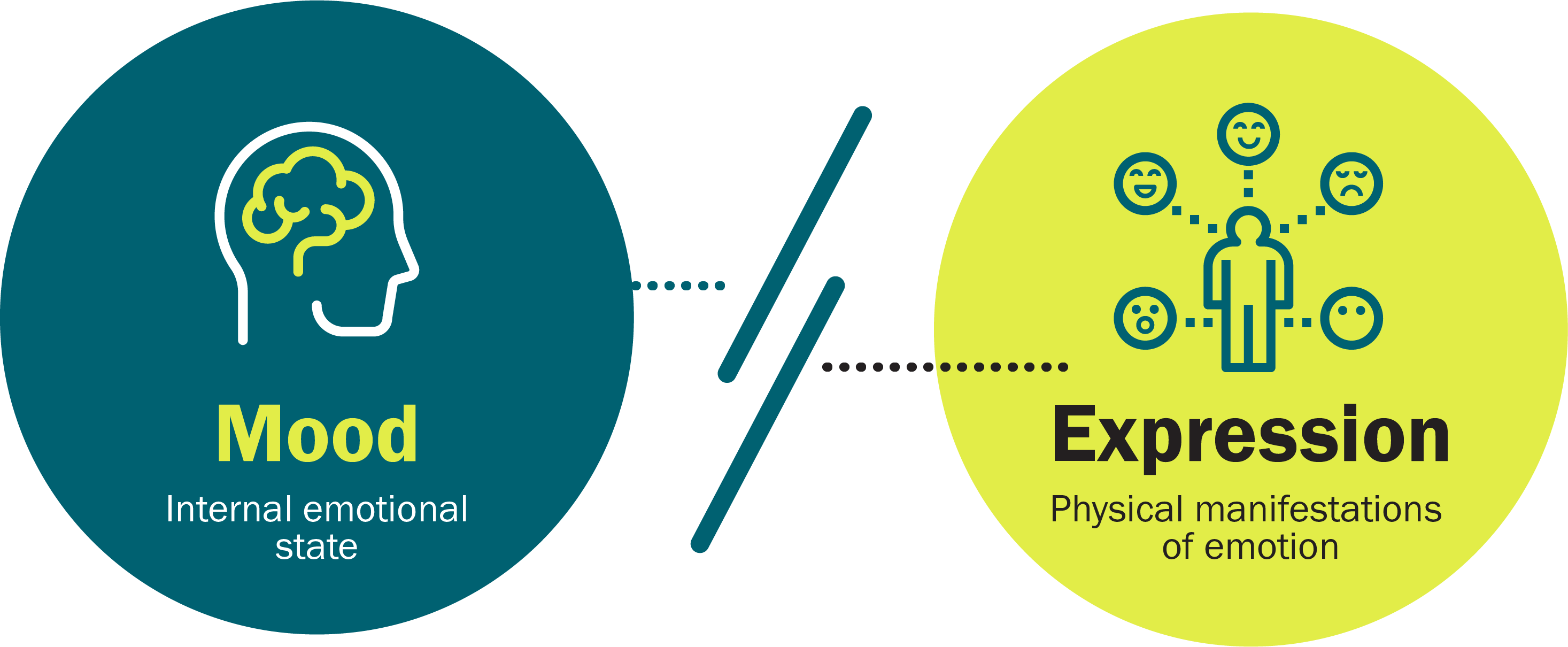
It is important to understand that PBA is a neurologic condition, not a psychiatric condition like depression, although PBA symptoms can be similar. With PBA, there is a disconnect between mood (how you feel) and expression (physical manifestation).
Finding a Specialist Who Treats PBA
If you think you have PBA but have not yet been diagnosed, it’s important to talk to a specialist. Not all healthcare providers are familiar with PBA, but doctors who specialize in treating neurologic conditions and traumatic brain injuries may have experience in treating PBA.
Hear About PBA Symptoms From Real Patients
“My crying episodes weren't matching what my body was saying or doing or feeling.”
— Sequena, a stroke survivor living with PBA
Individual results vary.
PBA Is More Common Than You Think
PBA is thought to affect about 1.8 million people in the US who suffer from certain neurologic conditions or brain injury.*† However, PBA is underrecognized and many patients remain undiagnosed.
Below is the estimated percentage of people with common neurologic conditions who have PBA symptoms:


*When considering patients with any of 6 common neurologic conditions associated with PBA, it is estimated that 37%, or an estimated 7.1 million Americans, have symptoms suggestive of PBA as defined by a CNS-LS (Center for Neurologic Study-Lability Scale) score ≥13 and 9.4% of patients, or an estimated 1.8 million Americans, with CNS-LS scores ≥21. The presence of PBA symptoms was defined as a CNS-LS score ≥13 and a more restrictive definition was also evaluated using CNS-LS ≥21. The CNS-LS was validated as a PBA screening tool in ALS and MS populations. A CNS-LS score ≥13 merits further diagnostic assessment.
†Common neurologic conditions included Alzheimer disease or dementia, ALS, MS, Parkinson’s, stroke, and TBI.
ALS=amyotrophic lateral sclerosis; MS=multiple sclerosis; TBI=traumatic brain injury.
Conditions That Can Cause PBA
Some patients who have had a traumatic brain injury may develop symptoms of uncontrollable crying and/or laughing very soon after their injury. For others, these symptoms may not be recognized until months after their TBI, during the recovery process.
Stroke survivors can experience emotional and behavioral changes during their recovery that can make it difficult to identify PBA symptoms as a separate condition. Also, because patients are often concerned with regaining lost function—and preventing another stroke—it may be easy to overlook uncontrollable crying and/or laughing symptoms or mistake the symptoms for depression.
Multiple sclerosis patients may experience a disruption in nerve transmissions throughout the body, producing a wide variety of symptoms that can be unpredictable and require different medications to treat them. This can make it challenging to diagnose PBA, as people with MS who develop uncontrollable crying and/or laughing episodes may not always know what’s causing them.
Alzheimer disease and other dementias can make PBA especially hard to spot, since sudden episodes of crying and/or laughing can be mistaken for depression or other personality changes associated with dementia.
While the main symptom of amyotrophic lateral sclerosis is gradual loss of motor movement, secondary symptoms can occur, including uncontrollable crying and/or laughing. PBA episodes can occur at any time for patients with ALS and may be mistaken for depression.
Parkinson’s disease is a progressive condition known for its physical symptoms, but it also affects areas of the brain that control emotional expression. While it’s important for these patients to address their physical symptoms with a doctor, it is also important to mention any changes in your crying and/or laughing, as it may be a result of PBA.
PBA and the Brain
The uncontrollable crying and/or laughing episodes of PBA may be a result of brain damage caused by neurologic conditions or brain injuries.
The parts of our brain that normally control emotional responses are the cerebral cortex and the cerebellum. Damage to the cerebellum, from a neurological condition or brain injury, may lead to miscommunication with the cerebral cortex. This miscommunication is thought to result in PBA episodes.

The Impact of PBA
Learn about how PBA can affect a patient’s day and the importance of an accurate diagnosis and treatment.
Mary-Beth is a real patient living with PBA. Image reflects patient’s health status at the time the image was captured.


Ready to Take the PBA Quiz?
If you think you or someone you love might have PBA, take the PBA Quiz to learn if the symptoms suggest PBA.
Liyah is a caregiver for a real patient living with PBA. Image reflects patient’s health status at the time the image was captured.



